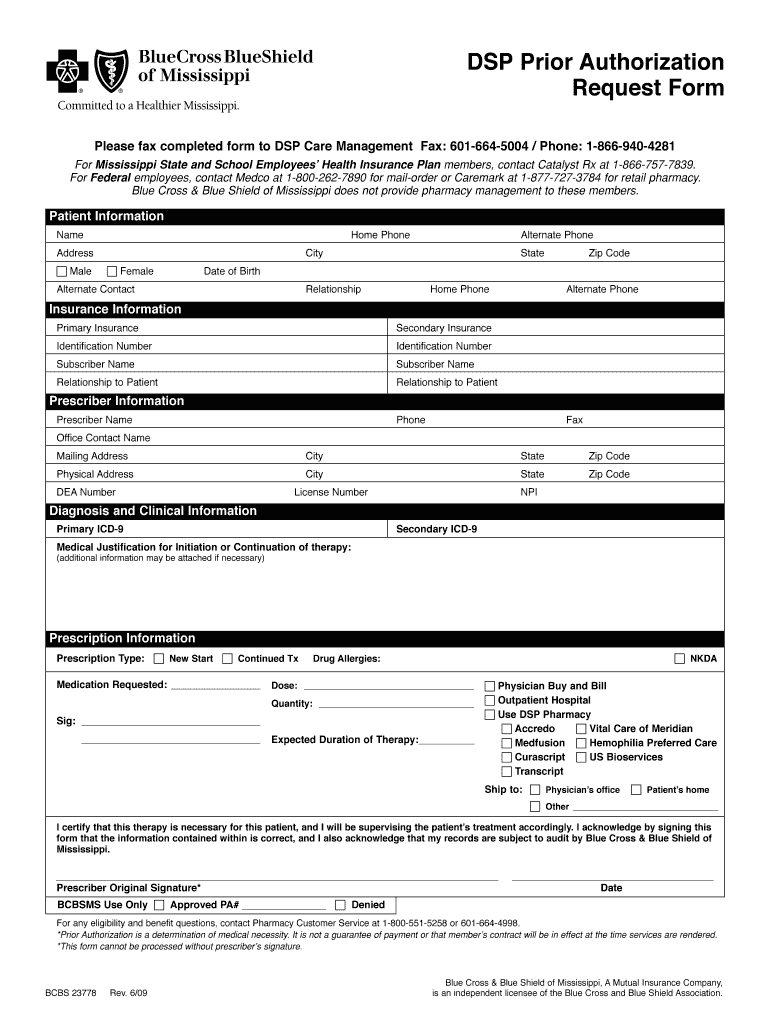
Blue Cross Blue Shield Of Mississippi Prior Authorization Form
Blue Cross Blue Shield Of Mississippi Prior Authorization Form - Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. If you are a mississippi network provider, you should submit your prior authorization requests. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prior authorization status please start the request by providing the following provider and patient.
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Prior authorization status please start the request by providing the following provider and patient. If you are a mississippi network provider, you should submit your prior authorization requests. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires.
If you are a mississippi network provider, you should submit your prior authorization requests. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Prior authorization status please start the request by providing the following provider and patient. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and.
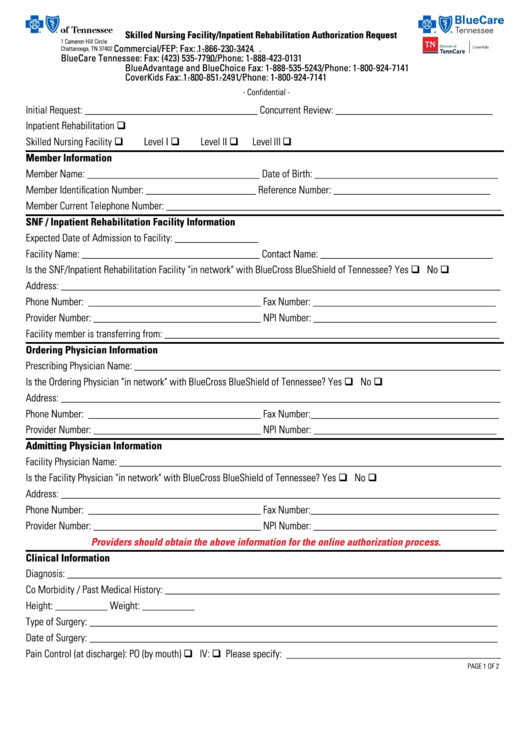
Blue Cross Blue Shield Of Massachusetts Prior Authorization Form
Prior authorization status please start the request by providing the following provider and patient. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. If you are a.
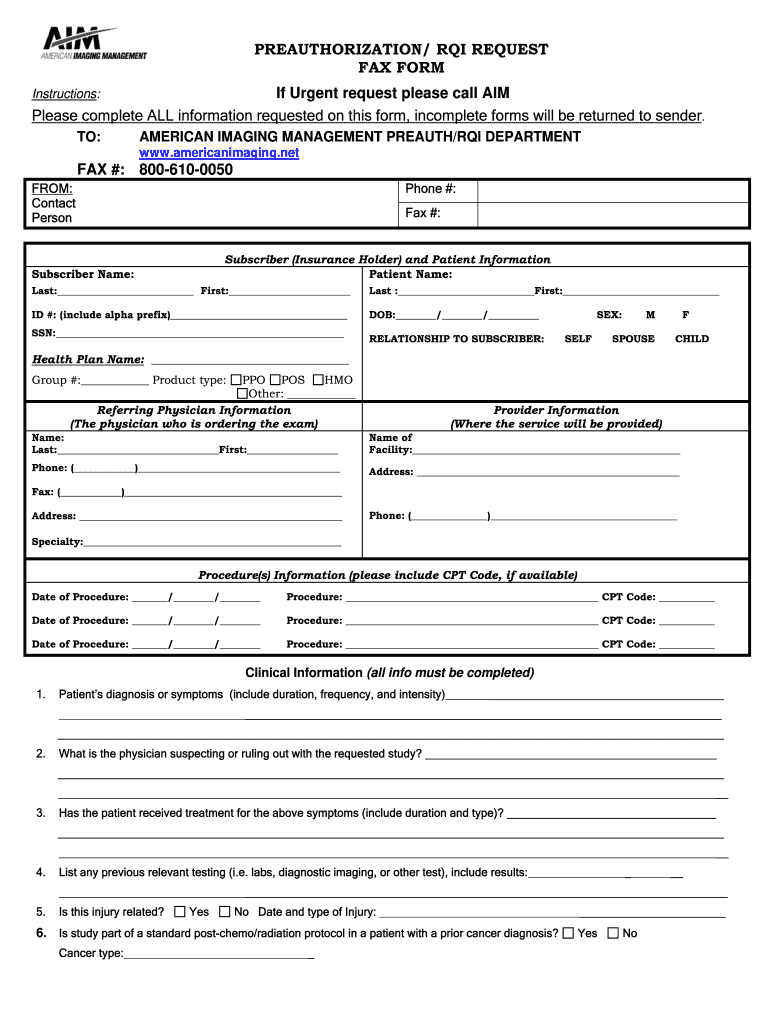
Fillable Online Blue cross blue shield prior authorization form pdf Fax
Prior authorization status please start the request by providing the following provider and patient. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. If you are a mississippi network provider, you should submit your prior authorization requests. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. All disease specific drugs must.
Bcbs mississippi Fill out & sign online DocHub
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. If you are a mississippi network provider, you should submit your prior authorization requests. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prior authorization status please start the request by providing the following provider and patient. All disease specific drugs must.
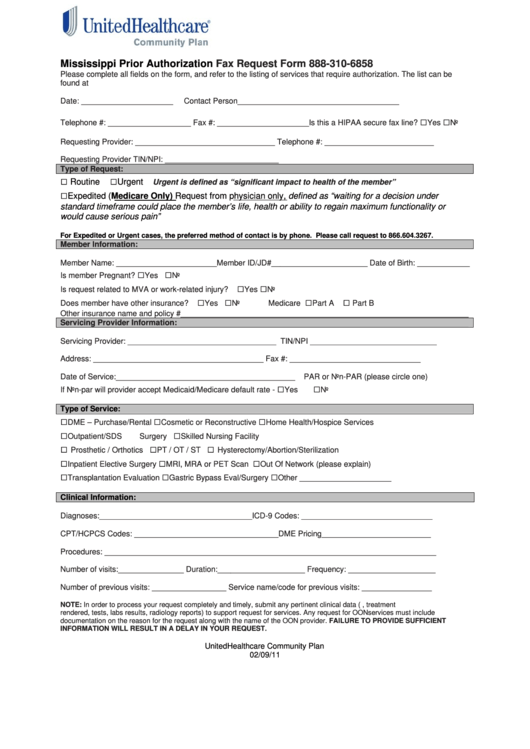
Mississippi Bluecross Form Fill Online, Printable, Fillable, Blank
All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. If you are a mississippi network provider, you should submit your prior authorization requests. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Prior authorization status please.
Blue Cross Blue Shield Sleep Study Authorization Form Study Poster
If you are a mississippi network provider, you should submit your prior authorization requests. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prior authorization status please start the request by providing the following provider and patient. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. All disease specific drugs must.
Fillable Mississippi Prior Authorization Fax Request Form printable pdf
All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Prior authorization status please start the request by providing the following provider and patient. If you are a mississippi network provider, you should submit your prior authorization requests. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Certain drugs must be prior.
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates free
If you are a mississippi network provider, you should submit your prior authorization requests. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Prior authorization status please start the request by providing the following provider and patient. Certain drugs must be prior.
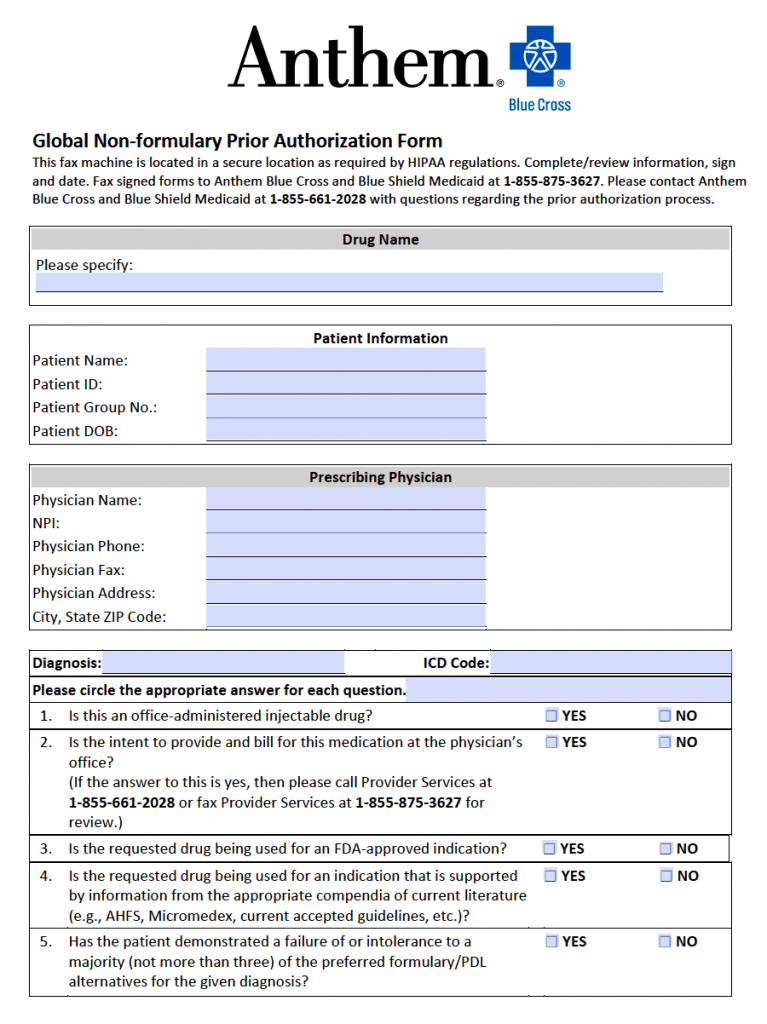
Free Anthem Blue Cross / Blue Shield Prior Prescription (Rx
All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Prior authorization status please start the request by providing the following provider and patient. If you are a.
CA Blue Shield Prior Authorization Request Form Resonance
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. If you are a mississippi network provider, you should submit your prior authorization requests. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Prior authorization status please start the request by providing the following provider and patient. Certain drugs must be prior.
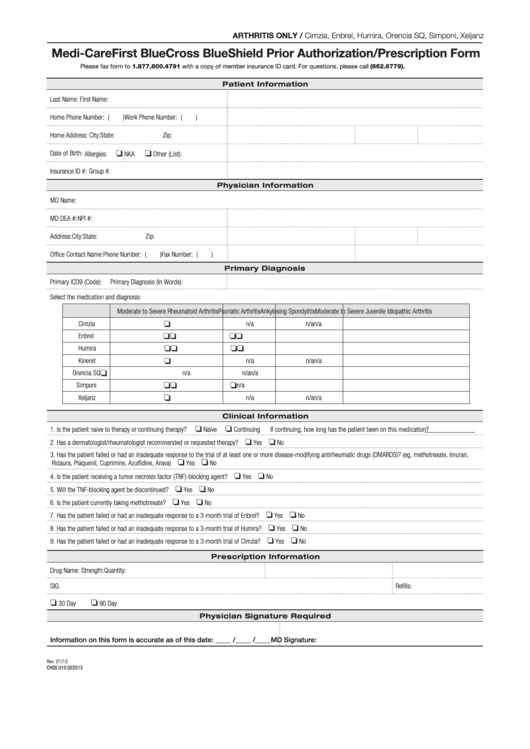
Fillable Medicare First Blue Cross Blue Shield Prior Authorization
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prior authorization status please start the request by providing the following provider and patient. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. If you are a.
Certain Drugs Must Be Prior Authorized By Blue Cross & Blue Shield Of Mississippi, And.
All disease specific drugs must be prescribed by a network provider, prior authorized by blue. If you are a mississippi network provider, you should submit your prior authorization requests. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Prior authorization status please start the request by providing the following provider and patient.